https://habr.com/en/company/klinika_shilovoy/blog/510892/- Клиника офтальмологии доктора Шиловой corporate blog
- Biotechnologies
- Health
Among the eye diseases are those that are especially dangerous. At first they are asymptomatic — nothing hurts, there are no complaints, they can “disguise” as other “mild” diseases and, most importantly, appear at any age and irrevocably “destroy” their eyesight.
Imagine if you left your left eye accidentally, but with your right, everything is “like a fog”! Read on the Internet how to help yourself or call your friends, and they — do not worry, blink. While they were waiting, it seemed that the fog was really over. This is how periods of anxiety recur, but at first there is little concern. And he (the murderer) began his insidious business. And as a rule, in both eyes, even if the second does not bother! And age is not an obstacle — children are also susceptible to this disease — 10% of children are blind from glaucoma.
Glaucoma is quite common in all countries — in 15% of cases of blindness, it is she who is the cause. This puts her in second place to the causes of incurable blindness!
And all is why — because the human brain very well «replaces» the dips in the field of view, if they arise gradually, adapt, and only when 30-40% of the optic nerve the feeling of «fog» begins. And all — hello, lost non-renewable!
Glaucoma — what happens?
The term glaucoma goes back to 400 BC, the so-called Hippocrates. First, it needs to be distinguished from cataracts — it talked about it here:
Cataract: it is waiting for you personally (if you live, of course)
In Hippocratic works “glaucosis” (Greek “become light blue”) and “hypochyma” (“clouding lens and its transformation into a gel-like mass ") these diseases are synonymous. Their separation occurred after 1705 — glaucoma became an incurable disease, and hypochime (cataract) was treatable. Do not believe it, but nowadays a huge number of patients come to our clinic with a diagnosis of «cataract», but in fact glaucoma is to blame for this. So God forbid to get to the clinic to a doctor with the level of knowledge of Hippocrates!
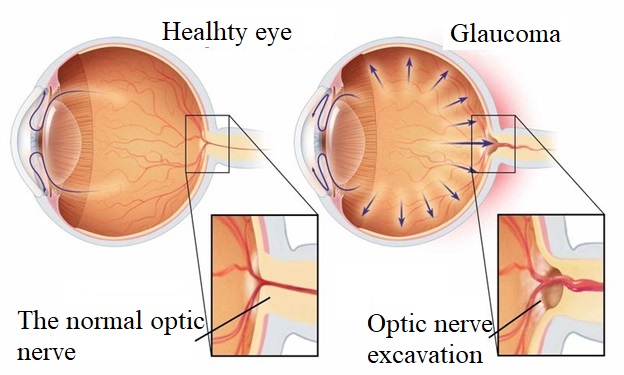
The cause of glaucoma is an increase in intraocular pressure as a result of disturbed outflow of intraocular fluid, its accumulation in the eye cavity and, as a result, atrophy of all intraocular structures and, most importantly, of the optic nerve. Specific atrophy, typical only for glaucoma, with the deflection of nerve fibers in the cranial cavity — the formation of an escalation-deepening. This is accompanied by losses in the peripheral visual field at the beginning, which are invisible to humans and the narrowing of the visual field to a “tubular” in a developed stage.
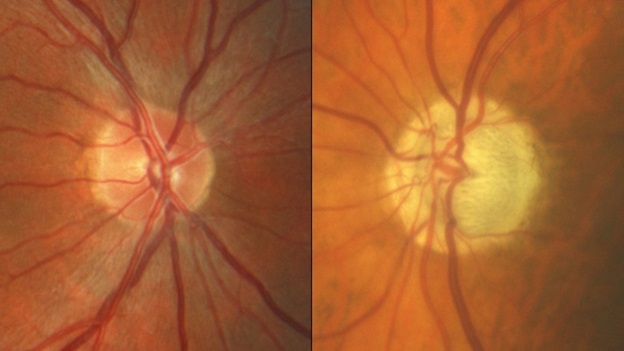
This is what an escalation looks like — this is the part of the optic nerve that the doctor sees through the pupil in the eye cavity.
Normally, intraocular pressure averages 15–22 mmHg. Art. But for each person, the rate indicator is individual and may be lower and higher than average values. With glaucoma, it can reach 80 mm Hg. Art. and more.
How the eye drainage system works
In the eye, all structures are “washed” by an intraocular fluid, which differs in composition from the blood — there are no red blood cells (red blood cells) in it and it looks transparent. It contains about 99% of water and a very small proportion of proteins, glucose, vitamins, hyaluronic acid, enzymes and trace elements. The composition and amount of moisture affects not only the life support of the avascular tissues of the eye, but also the stability of the level of intraocular pressure.
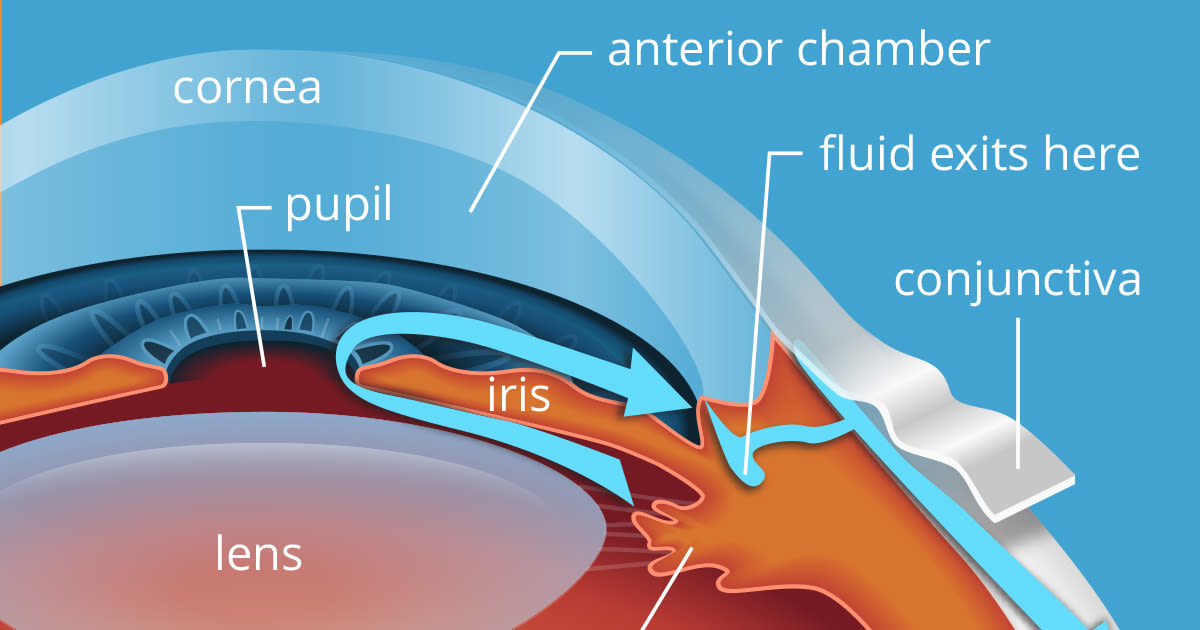
The movement of fluid occurs with the direct participation of the lens and vitreous body: intraocular fluid is continuously produced by the processes of the ciliary body, accumulates in the posterior chamber, which is a slit-shaped space of complex configuration, located posterior to the iris. Then most of the moisture flows through the pupil, washing the lens, and then enters the anterior chamber and passes through the drainage system of the eye, located in the zone of the anterior chamber angle — the trabecula and Schlemm's canal. From it the intraocular fluid flows through the outflowing collectors into the superficial veins of the sclera.
Schematically it looks like this:
The front wall of the anterior chamber angle is formed at the junction of the cornea in the sclera, the back wall is formed by the iris, the front part of the ciliary body serves as the apex of the angle.
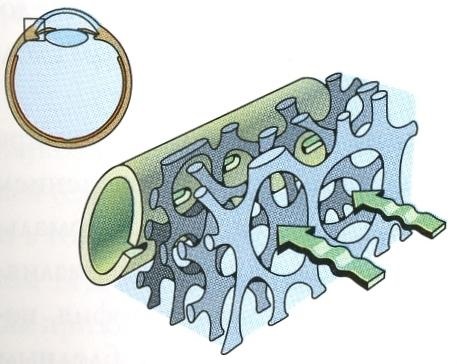
That is, the aqueous humor (fluid inside the eye) seeps through the ring in the form of a grid with a multitude of slots and openings and collects into one main canal — the Schlemmish canal — 0.3–0.5 mm in diameter, and then, after 25–30 thin tubules, goes to the outer veins.
ТTrabecular apparatus is a multi-layer, self-cleaning filter that provides one-sided movement of fluid from the anterior chamber to the external veins.
The described path is the main one and 85-95% of the aqueous humor flows through it.
The outflow of aqueous humor is disturbed for several reasons. They determine the type of glaucoma and the effective method of treatment for this type.
With angle-closure glaucoma (only 20% of all cases), the iris closes the exit from the chamber of the eye, preventing the exit of fluid.
In open-angle glaucoma (the remaining 80%), there is a violation in the capillaries themselves, into which the fluid must fall (blockage, compression).
Glaucoma can appear as an independent disease — then it is called primary, and it can occur as a result of other diseases — then it is secondary. Secondary glaucoma appears after injuries (sometimes minor), falls, inflammations in the eye, while taking certain medications (for example, hormones), etc.
What can say about glaucoma?
First, rainbow circles in front of light sources. The so-called «halo» effects. They appear due to corneal edema with increased intraocular pressure.
Secondly, the appearance of «turbid» spots in the lateral (peripheral) or central field of view is possible. «Muddy» spots, or scotomas, are «dropped» areas of the picture before the eyes. They may appear as dark or blurred dots and spots that do not disappear after blinking and remain permanently in the same place. A person begins to see worse first around the periphery of the visual fields.
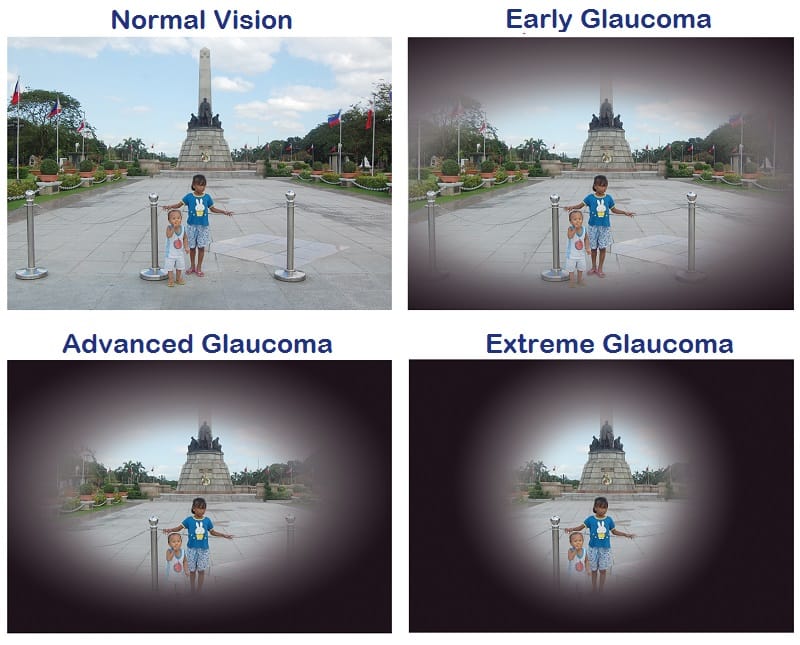
Tunnel vision appears in advanced stages. It looks like a circular limitation of the field of view, as if you are looking through a sheet of paper rolled into a tube.
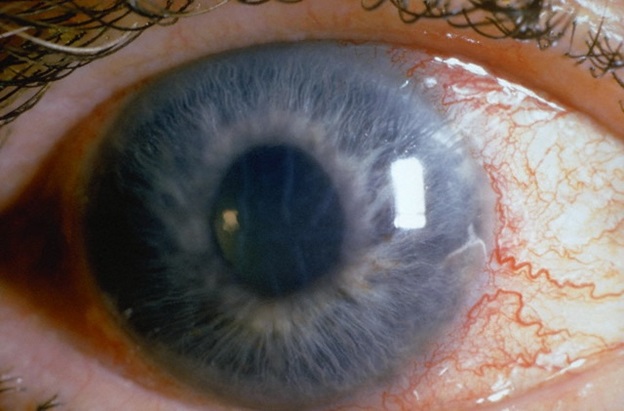
Third, the redness of the eyes. In case of glaucoma, a grid of dilated red vessels may be clearly visible against the background of the white of the eye. Especially strongly it is visible with very high intraocular pressure or acute attack of glaucoma.
Fourth, the severity and pain in the eyeballs, sometimes until nausea and vomiting. Such manifestations in glaucoma are usually provoked by a strong pain syndrome.
Fifth, there may be a feeling of dryness in the eyes and discomfort, increased tearing and photophobia.
How not to blink glaucoma?
It is impossible to make a diagnosis on your own — the symptoms are very similar to other diseases.
The initial glaucoma can be determined only by a competent specialist with sufficient equipment with modern diagnostic devices. How to find such a specialist — only in the eye centers, where they are engaged in glaucoma. City Clinic for this is suitable.
A full examination requires a lot of time — sometimes up to 1-2 hours and a whole range of instruments, the results of which are evaluated together: visometry with and without correction, perimetry, biometrics, tonometry, tonography, gonioscopy, pachymetry, ophthalmoscopy, computed tomography of the optic nerve, fluometry, laser scanning topography.
Here is such a big set of studies! And, very importantly, the eye is a paired organ, and it is necessary to examine both eyes at the same time, not because the ophthalmologists want to cash in on you, but for the accuracy of the diagnosis.
And, last but not least, these examinations need to be repeated over time, both when glaucoma is suspected (to make a diagnosis), and for certain glaucoma (to determine the pressure of the “target” and control the progression of the disease).
In our clinic, complex diagnostics in such a volume costs 7,500 rubles and takes about 1-1.5 hours. But it is definitely worth it, because late diagnosis and delayed prescribed treatment lead to irreversible consequences.
What is “target pressure”?
As a person is not a serial sample, each has its own anatomical nuances and its own standard of intraocular pressure. For example, the smaller the thickness of the membranes of the eye (and this is more often in short-sighted people), the more likely the tissues and nerve endings wear out: a balloon withstands completely different pressure than a football. Therefore, the absolute values of intraocular pressure do not make sense, because we are all so unique that for one 15 mm Hg. Art. already a lot, but for another the rate of 25 mm Hg. Art.
Intraocular pressure has an individual value for each person and is diagnosed in dynamics, in comparison with a healthy eye, in relation to the previous indicators.
Who needs to be diagnosed right now?
- Firstly, if you are over 40. Although glaucoma can also occur in children, it is rather an age-related ailment.
- If the family were relatives with glaucoma. Alas, the genetic propensity for this disease is inherited along with her grandmother's apartment.
- Myopic people are more often prone to glaucoma, because they have thin eye membranes and glaucoma develops faster and more aggressively than the average person.
- If you notice the above symptoms. You should not carry out the prevention of vision, eating blueberries with buckets — this is lost time and a direct road to blindness.
Comprehensive survey for glaucoma — what are the features?
Tonometry
The measurement methods are different. Since you cannot put a manometer in your eye — all measurements are indirect, based on the response of the cornea to compression. Hence the error.
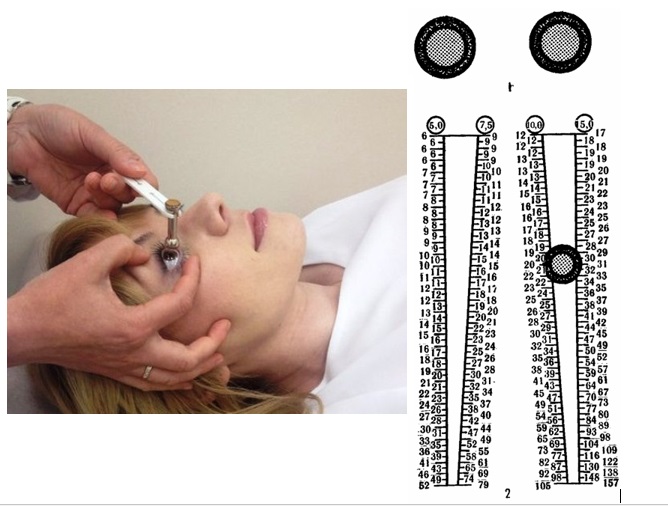
Because it depends a lot on the cornea itself — its thickness, curvature, state, on the way of pressing — by air or a weight, on the patient's behavior during the measurement, and, of course, on the correctness of the operator. By the way, the method of measuring intraocular pressure according to Maklakov is still being used today, which is quite accurate with proper execution: a weighted paint is put right on the cornea after the “freezing”, then removed and applied to the piece of paper to estimate the imprint diameter. The higher the pressure, the harder the eye and the «contact patch» less. The print is measured manually by a ticker.
And this is how pneumotonometry looks like:
However, if you have increased blood pressure, this is not a guarantee of glaucoma. Raising can be temporary. For the accurate diagnosis of glaucoma, other examinations are prescribed.
Gonioscopy is an examination of the anterior chamber angle of the eye. The procedure allows to determine the type of glaucoma: open-angle or angle-closure and the condition of the primary eye collector. After the “freezing”, a special 4-mirror contact lens-gonioscope is applied to the eye and the doctor has the opportunity to see the hidden eye zones — the angle of the anterior chamber and Schlemm's canal.
With the help of tonography (research of hydrodynamic functions of the eye), it is possible to assess the cause of the pressure increase — either more fluid is produced than needed, or outflow is difficult. This affects the choice of treatment. Not the most pleasant examination — a small weight is put on each eye after the “freezing”, certain values are calculated and compared with the norm — minute volume of chamber moisture, lightness factor of outflow, true intraocular pressure, etc.
Determination of visual fields — perimetry
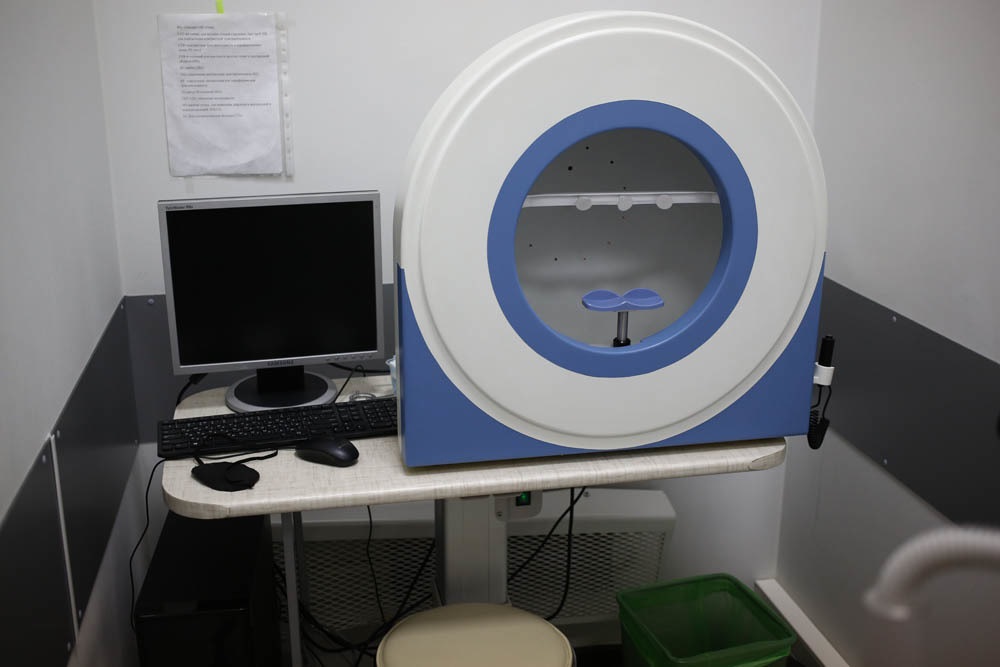
Computer perimetry: the device for perimetry looks like a big white hemisphere with a face stand with a computer connected to it.
It is necessary to close one eye, and the second to look strictly forward. By the way, in modern perimeters, the operator monitors the camera for the correctness of the position of your eye. If you notice a blinking light with side vision, you need to press the button — “flash to the right”. As a result, a diagram of the visual fields for each eye is drawn up. There are special screening programs for detecting glaucoma, in which flashes are generated with a given frequency and different wavelengths. Dynamics of glaucoma:
By the way, you can distract from the code and check your peripheral vision in the old-fashioned way with your colleague: sit face to face, one will cover your left eye with your hand, the right eye with the other. Then, gently looking at each other's eyes in the eye — this is important — one of you pulls his hand to the side. If someone has peripheral vision deteriorated, then for him this hand may be invisible.
In the same way, check the peripheral vision in the other eye, not only in the horizontal, but also in the vertical plane. If in some areas «failures», it's time to run to the doctor.
But back to more accurate research methods.
OCT — optical coherence tomography
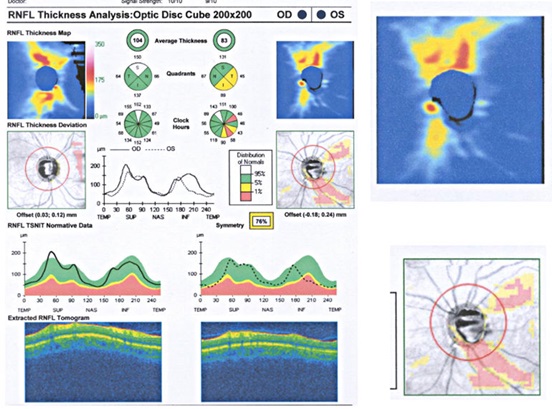
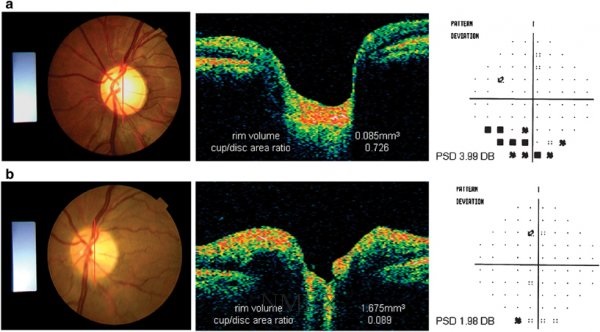
The next stage of diagnosis is the determination of the state of the optic nerve. From pressure, it begins to «fall» deep into the skull, glaucomatous excavation appears. In advanced stages, a doctor can see signs of glaucoma with a simple ophthalmoscopy. But the “gold standard” of the examination of the optic nerve today is optical coherent tomography and laser scanning topography. And, once again, the survey should be done in two eyes.
We estimate such morphological parameters of the optic nerve head (head).
And here is a picture of the assessment of the ganglion cell layer, primarily those suffering from glaucoma — the norm on the right, glaucoma on the left:
This is how the fundus picture correlates with tomography of the optic nerve head and perimetry (glaucoma — above).
Such measurements allow you to diagnose glaucoma at the earliest stages and to conduct very accurate dynamic observation.
If at this stage you do not see a doctor and do not start treatment, after a certain time, the same changes will occur in the second eye. With further progression of glaucoma, the visual field will decrease until the person is completely blind.
How not to allow glaucoma to accomplish its “black deed”? About this in the next post