https://habr.com/en/company/klinika_shilovoy/blog/502144/- Клиника офтальмологии доктора Шиловой corporate blog
- Biotechnologies
- Geek health
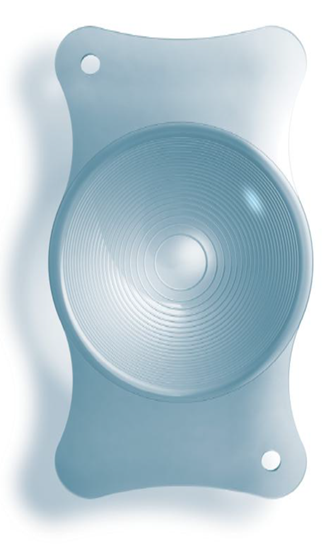
 This is a model of an intraocular multifocal lens from Carl Zeiss. The real size of such a lens is 11 millimeters, the diameter of the optical zone is 6 mm.
The cataract is, simplifying, age opacification and consolidation of a crystalline lens.
This is a model of an intraocular multifocal lens from Carl Zeiss. The real size of such a lens is 11 millimeters, the diameter of the optical zone is 6 mm.
The cataract is, simplifying, age opacification and consolidation of a crystalline lens. According to the classical definition, we are talking about the turbidity of any type. First, something gets in the field of view, a general “fog” appears, you want to wipe dirty glasses, then you do not see the letters in the book, then you want to turn on the light brighter or, on the contrary, you hide from the bright light, and then wake up one fine morning and understand that you can not find slippers. And you see nothing at all — only the shadows. This process sometimes stretches for many years, but slippers are still lost. Mention of clouding that develops in the eyeball, there are still thousands of years before our era.
The treatment procedure has historically been very peculiar — reclination of a cloudy lens. The doctor took the patient with a very dense lens — to that dense stage that the patient is already blind. During the excavations of the settlements of ancient Greece and Rome, the tools used by doctors to remove cataracts were found — sharp needles that pierced the eye and lens, destroying its supporting apparatus. The lens could come off and, by virtue of its gravity, could also fall down from hitting the back of the head with a heavy stick several times. Sometimes the patient died during the emergency eye care, sometimes he had a concussion, and sometimes the lens fell off the ligaments and flew deep into the eye. The patient began to see again — he had a huge lump and vision of about +10 +15 diopters.
Now two news. The bad — people began to live to cataracts more often, and it is inevitable. Good — we have something better than sharp needles and a heavy stick.
What happens to the lens with age
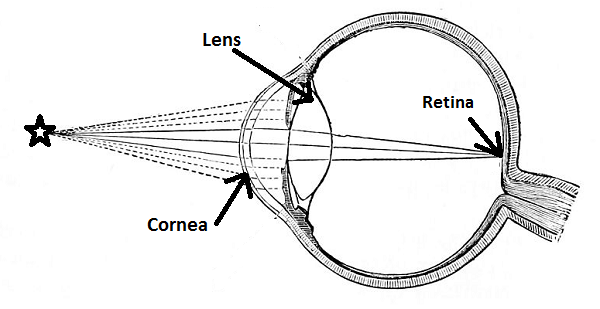
If you read the previous posts, you already know the cornea. This is the first strongest refracting lens of the eye, it is formed by about 16–18 years old and changes slightly during life. Then we have the second “group of lenses” — lenses (lens — natural lens in English terminology). And already behind him, through the vitreous body — the sensor, that is, the retina.
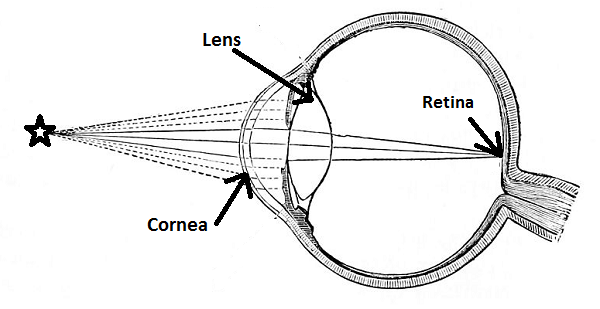
The lens is responsible for the refraction of light (about +20 diopters at rest and about +30 diopters under voltage) and focusing the eye. When we look at a book, the muscles tighten and shape it so that the focus falls on the letters. When we look at the plane in the sky, the muscles relax, and the lens forms almost parallel rays. Muscles are not located in the lens itself, but in the zone of the so-called ciliary body, lens bundles are attached to them, which, in turn, allows accommodation, that is, this fine adjustment to the desired focal length by changing the shape of the lens. If you get the lens at all, you will see with glasses somewhere between +10 and +15 diopters.
With age, the lens gradually becomes dense and grows turbid. A young man in the lens usually has only 60–65% of water in the tissues. In old age, the amount of fluid decreases. Although the lens «floats» in the liquid, it is relatively dry. On the other hand, in the crystalline lens itself, due to its structure and the absence of vessels, there are no tumor or inflammatory processes. The lens does not hurt, because there are no nerve endings in it.
Often, a cataract as it develops causes a weakening of presbyopia and the possibility of reading without glasses, that is, two age-related pathologies suddenly correct each other. But this is an imaginary improvement in vision, while the image quality is poor — this is a sign symptom of cataract development.
At about 60–70 years old, the lens completely loses the ability to accommodate, that is, it becomes rigid, large and inelastic. Even the lens turns yellow with age.
Yes, I must say that cataract is not necessarily an age-related phenomenon. There are congenital cataracts (if during pregnancy a woman suffers from some infectious, systemic or genetic diseases).
There are complicated types of cataracts that appear in case of concomitant diseases of the eye or the whole organism, for example, diabetes, arthritis, etc. Taking certain medications also causes cataracts.
And, of course, any injury to the eye can cause the appearance of a cataract, even if there was no direct contact with the lens. It is now known that cataracts are caused by strong infrared radiation, as well as various radiation factors, and not immediately, but years later. This, in particular, calls into question the use of powerful lidars of unmanned vehicles operating in the IR spectrum — until their influence on the eyes in the long term has been studied for several years. It is also known that the current of ultrahigh frequencies also leads to the development of cataracts. Another cataract can cause poisoning, in particular (very characteristic) nitrokraska. In animals, cataracts have learned to predictably get mothballs and specific diets.
But back to the usual age-related cataract. A very characteristic symptom of the process that has begun — it seems to the patient that he has “dirty” glasses, and there is a constant desire to wipe them off. If you suddenly notice this for an elderly relative — it means that it’s time to exactly change the lens.
Sometimes patients misinterpret the symptoms that appear. Very often, a cataract matures by condensing the lens — along the sclerotic path. In this case, a patient with a cataract, who read with glasses, suddenly begins to notice with surprise that they now see poorly and the opportunity has appeared, albeit in a «fog», but to read the text without glasses. The patient feels joy and thinks that he has begun to see better. Alas, this is a bad symptom! He says that you need to plan a visit to an ophthalmologist.
Often a cataract leads to the fact that myopia, which has been stable for years, suddenly begins to increase. Sometimes up to huge values - in –20 diopters and more. In general, the frequent change of glasses is an early sign of the appearance of cataracts.
The second variant of cataract maturation is no better — hydropic, when the lens begins to increase in volume, it hydrates, swells and leads to an increase in intraocular pressure and rapid loss of vision.
There are still a number of symptoms: in the twilight it becomes better to see what the rainbows and ghosting disturb you during the day, astigmatism appears or increases. In general, a cataract is very diverse in its manifestations, it is impossible to make a diagnosis on your own, for this you need a visit to an ophthalmologist.
When is the lens removed?
There are three types of indications for the replacement of the lens: optical, refractive and medical.
Optical readings are when aging and compaction of the “bulb” in layers has reached the logical end and the lens darkens. Then, when the cataract begins to reduce vision qualitatively or quantitatively. Sensations — as if smoked glass were inserted into the eye or as if you were looking at the world through glass splashed with semolina. Even the initial cataract, which is the cause of reduced vision requires removal.
The old term “immature” is no reason to wait for ripening. The diagnosis of «cataract» — a reason to replace the lens.
When a person no longer sees objects and only light perception remains, this is the last stage of a mature cataract. It is better not to bring it up, in particular, because a change in the lens causes numerous disruptions in the normal functioning of the eye. In mature and over-ripe forms, the lens capsule, ligamentous apparatus suffers, removal requires a large amount of ultrasonic energy, which, in turn, destroys the cornea, its delicate endothelial layer. In general, if you pull with the replacement of the lens, you should be prepared for the fact that the operation will be longer and more traumatic, with a long recovery period.
Refractive indications — change in optics of the eye. By replacing the lens and correct calculations of the optical power of the implantable artificial, we can change the refraction of the eye to the desired value — save the patient from a large «minus» or «plus», correct astigmatism, save from age long-sightedness. In this case, the cataract does not develop, and the optics of the eye remains stable forever.
Most often, this method is used for patients older than 40-45 years old when the first symptoms of presbyopia appear.
Medical indications — this is when your own lens is the cause of concomitant changes in the eye, for example, when there is subluxation after injury and there is a risk of its dislocation, when it is the reason for the formation of glaucoma (dangerous increase in intraocular pressure and death of the optic nerve), etc. That is, again, simplifying, the lens will sooner or later change anyway, but because of the risk of pathologies, sometimes it needs to be changed a little earlier than it develops a resource.
Do I have to wait until the patient is completely blind?
Patients often use this logic: while the eye sees something, it is not necessary to operate the lens. In fact, today, on the contrary, the lens is operated as early as possible, when it is already clear that the irreversible process has begun. The reason — apart from protecting against the risks caused by changes in the metabolism in the eye, is that the softer the lens is at the time of the operation, the less invasive the method will be, and the less the risk of complications.
The generalized global risk of severe and serious complications of a lensectomy fluctuates around 6%. In the case of late stages, it can reach up to 20–30%. In the early stages, this is 1–2%. In the case of the use of modern equipment for access, a very precise selection of the lens-implant itself and more than 5 years of experience of the surgeon — less than 1%. What so strongly influences the risks, I will tell in the next post, when we talk directly about the course of the operation.
Another important point is that you yourself will never be able to independently determine the condition of your lens. There are a number of factors that force surgeons to advise the operation at an earlier date: a weak ligamentous apparatus of the lens, short or, on the contrary, long eyes, eyes with a shallow anterior chamber, the state of the corneal endothelium, and other things that only a specialist who performs this operation can assess type Quite often, outpatient physicians act as advisers, who are not always well versed in the technique of operation and the indications for replacing the lens. Calming the patient with the words “you have an immature cataract, it’s too early to be operated on”, provide the patient with a “disservice” service — inaction leads to when the optimal time is missed.
In general, cataract surgery in ophthalmology is like appendicitis surgery in general surgery. It is considered the most basic and most predictable in the standard case, the most creative in the non-standard case. If everything goes according to the scenario, even an inexperienced surgeon will have a good result. If something goes wrong (and this cannot always be predicted in advance), then only an experienced surgeon can find a way out of a non-standard situation. I have very often, almost weekly, to do reconstructive operations after unsuccessfully performed operations in other clinics. Sometimes the volume of such surgery is huge — operations lasting not 10–15 minutes (as with a standard cataract), but 1–2 hours of “creativity”.
An important point in cataract surgery is the choice of the lens. And the main factor is the consideration of the individual characteristics of a particular patient. IOL models (intraocular lenses) differ in the material of manufacture, the shape and number of supporting elements, the structure of the optics (spherical, aspherical, astigmatic), the method of attachment. Therefore, it is better to choose not American or German, “as a neighbor’s”, but one that your surgeon considers most suitable for your eye.
And the most important. Replacing the lens restores the transparency of optical media and can improve the optics of the eye, but it will not create a new eye. If there are concomitant problems with the retina, optic nerve, cornea or brain, then there are other problems for reducing vision, then they will ultimately determine how you will see after the operation. That is, postoperative visual acuity will be what you visual analyzer in general.
Where is the best operation?
The following is important: «planned» replacement of the lens is included in the OMC package. The patient always has the right to choose whether to go to the nearest territorial clinic for referral to a budget institution or to come to a clinic for diagnosis and surgery. The question «where is better?» There is no single answer. Everyone chooses, based on his life experience, advice from friends, financial situation, mobility and much more.
There is one piece of advice when choosing the OMC option: if you were offered to buy a lens or even all “consumables”, arguing that the hospital does not have lenses or something else, then you should be deceived. The MHI system does not involve co-financing, that is, if you receive a service under the MHI policy, then everything should be free for the patient, including lenses, solutions, etc. Or everything is paid. Two options. Partially — impossible. The amount that is transferred to the hospital for this service includes a payment for everything that is needed for this technology. And if you bought from a certain company (as a rule, according to the advice of your doctor, it was in a particular company “Horns and hoofs”), then where did the lens come in and get it for your operation? In regions this practice is rare, in large cities it is very frequent.
Otherwise, one should know that cataract operations do not require hospitalization and are performed on an outpatient basis. When using modern high-tech techniques last only 10-15 minutes, completely painless, have no age restrictions. After surgery, the patient almost immediately leads a normal life, for a month digging in drops in the familiar home environment.
Will the implant accommodate?
The term «accommodation» is applicable only to the natural lens. But if we expand the question to “whether an artificial monofocal lens will focus on different distances without additional correction with glasses,” the answer is no. It is adjusted to a specific focal length, the choice of which is always discussed with the patient. If a person has always seen the distance without glasses, and he needed reading glasses only after 45–50 years, then, as a rule, the lens is calculated for distance vision and for near in this case an additional correction with glasses with plus glasses will be required. If the patient was short-sighted and read without glasses, then you can stay in the residual myopia at -2 -2.5 diopters and glasses for distance.
For greater independence from glasses, in some cases the principle of “monovision” is used, when in the leading eye the optics are calculated on the distant focus, and in the non-advanced eye the calculation is made for near. This choice is always discussed with the patient and pre-tested.
There is a concept of the so-called “accommodation of a pseudofack eye,” that is, an eye with an artificial lens. This process involves not only the ligamentous apparatus, but also the vitreous body and the entire posterior pole of the eye, as well as the cornea. This process is unpredictable, and during the first year after the operation it is significantly weakened.
There is one more type of lenses that have multifocal optics that can create focusing at different distances without additional correction with glasses.
These are lenses that refract light with several foci, allowing you to see objects at different distances. Thanks to these lenses, patients receive maximum independence from glasses in their daily lives.
Along with age-farsightedness, artificial multifocal lenses can correct myopia, hyperopia, as well as astigmatism.
Trifocal lens is an advanced multifocal lens with an additional focus. It allows you to clearly see objects both near and far, and at an average distance. And the patient can easily work on the computer.
Since after the implantation of an artificial lens, the range of refraction of the eye will no longer change, so the patient can get rid of the glasses for a lifetime. The great advantage of life without glasses is associated with a slight decrease in the quality of vision in some areas. This is due to the physical principle underlying the design of multifocal and trifocal lenses, which constantly divide the light into the near, far and intermediate.
However, due to the high degree of light transmission of trifocal lenses, unwanted light scattering or light effects practically do not occur. Even with poor light it is possible to achieve very good refractive results. Variants of monofocal intraocular lenses. System for the implantation of an intraocular lens.

Monofocal intraocular lenses

Intraocular lens implantation system.

Astigmatic (toric) intraocular lens.
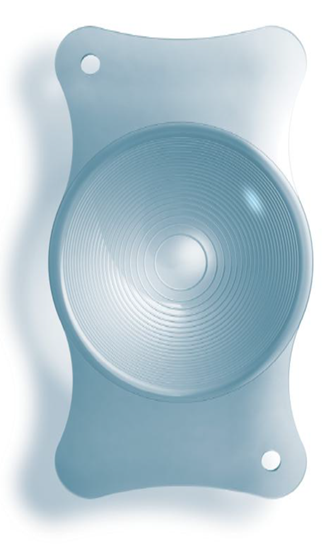
Multifocal trifocal intraocular lens.
After implantation of such lenses, adult family members often see their children, grandmothers, better than their grandchildren. Very often after that, they begin to complain that before the operation their own face and the faces of relatives were “younger”, complain that they have grown old, and rejoice in the long-forgotten colors of the world. Choosing a lens is always an individual task that you can only solve with your surgeon. Because the replacement of the lens is done once and for all, you do not need to change the lens during life.
The operation itself is in the next post.